Apparently USAID want to spend $24.5m on a mass male circumcision program in Swaziland, aiming to circumcise 150-200k males, including infants and others who are both too young to give their consent, and to be sexually active. There are three women infected for every two men, which makes one wonder why male circumcision is seen as the best way of spending this money. But for reasons best known to themselves, USAID and other institutions really want to spend money on mass male circumcision programs, even though they are destined to fail to reduce HIV transmission to any great extent, and may even increase transmission according to their own research.
The mass male circumcision program in African countries is predicated on almost all HIV transmission being a result of ‘unsafe’ sexual behavior. However, those who do not engage in such behavior will not be protected by circumcision. Researchers collecting figures for the Demographic and Health Survey suggest that some people may not report their sexual activity, which is as true in Swaziland as it is anywhere. But knowing someone is HIV positive does not tell you how they were infected. What about partner tracing? Were their partners tested? What about their non-sexual risks, such as unsafe healthcare, cosmetic and traditional practices? These are not as thoroughly investigated as people’s ‘unsafe’ sexual behavior, but without this information we can not know how they were infected. Even sexually active people are at risk of non-sexual transmission of HIV. Mass male circumcision will fail everyone at risk of being infected with HIV through non-sexual routes.
Aside from the fact that HIV prevalence among circumcised men is not that different from prevalence among uncircumcised men, about one fifth of men and almost one third of women aged 15-49 years are already HIV positive. Exactly how were all these people infected? It’s just assumed (by the HIV industry) that they must have been infected sexually. The 5.2% of women and 2.1% of men found to be HIV positive, but who said they had never had sexual intercourse, were also likely to have been infected by some non-sexual route.
The mothers of 11 out of 50 infants found to be HIV positive were themselves HIV negative, so those infants would have been infected through some other non-sexual route, probably through unsafe healthcare. Mother to child transmission (MTCT) is acknowledged as a non-sexual mode of transmission; it is even assumed when infants and young children are infected. But given the above mentioned findings, this assumption could easily be wrong even in some cases where the mother happens to be infected.
Mass male circumcision was introduced in Swaziland in 2007, targeting HIV negative men between 15-24 years and newborn babies (though it is available to all uncircumcised men). 13.3% of men in urban areas are already circumcised and 6.2% of rural men. Why is the practice less common in rural areas? The reason for the question is that HIV prevalence is higher in urban than rural areas and it would be interesting to know if sexual practices really are substantially different, or if conditions in and access to health services, health seeking behaviors and other, non-sexual circumstances were also different. Not many people would wish to be circumcised in health facilities where practices are unsafe, where they may be infected with the very disease the operation is said to avert.
It is reported that 43% of men between 15-49 years say they want to be circumcised, compared to 54% who say they do not. Saying you want to be circumcised is not the same as actually going ahead with the operation, as various mass male circumcision programs have already found. The use of the term ‘man’ is also suspect. How many children and people in their early to mid teens will also be railroaded into agreeing? Apparently the recruiters go to schools and press-gang whole classes to turn up to be circumcised in Kenya; once a few agree, all the others are afraid to refuse.
Rather pathetically, the Demographic and Health Survey finds that “the relationship between HIV prevalence and circumcision status is not in the expected direction”, meaning that prevalence is higher among circumcised men (21.8%) than uncircumcised men (19.5%), something that has been found in many countries. To be fair, the numbers of circumcised men are not high, so it’s hard to tell if the difference on its own deserves much attention.
A good deal of other potentially useful data about circumcision was collected, but not reported in the DHS Survey. For example, people were asked their reasons for circumcision, whether tradition/religion, health/hygiene, sexual satisfaction, ease of putting on a condom, other and don’t know. I suspect most people would have had it done, voluntarily or otherwise, for traditional or religious reasons because the health/hygiene arguments had yet to be manufactured when this report was completed; the increased sexual satisfaction argument is spurious and was also added in to the repertoire more recently; ease of putting on a condom, also entirely spurious, is relatively recent; one can only imagine what ‘other’ reasons may have been given, and why someone would choose to have a circumcision without knowing the reason, unless they had given in to peer pressure.
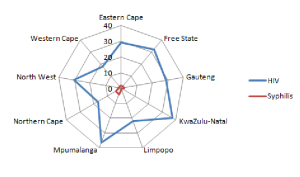
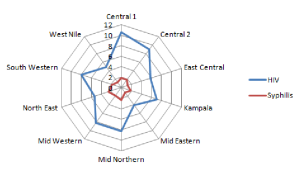
The Global Burden of Disease Report for Swaziland finds that HIV is the top cause of premature death in 2010, accounting for 41% of years of life lost, 341 per 1,000, an increase of 1,625% on the 1990 figures. But syphilis, which stood at number 7 in 1990, accounting for 3% of years of life lost, is no longer in the top 25. It fell further than any other disease over the 20 year period. Why is an easy to transmit infection like syphilis dropping in prevalence in a population said by the HIV industry to engage in high enough levels of ‘unsafe’ sexual behavior to result in the highest HIV prevalence in the world?
The list of reasons why mass male circumcision will fail, as will any other ‘intervention’ predicated on HIV being almost entirely sexually transmitted, goes on. Many people, probably a majority, only have one sexual partner; only a few have many. Most people don’t engage in ‘higher risk’ sex, though some do. Many people ‘take precautions’, though not enough. Factors such as residence, employment status, education level and wealth quintile are often said to determine people’s sexual behavior, but they also determine their health, health seeking behavior and many other things.
Even the sexual behavior data frequently contradicts assumptions about HIV being sexually transmitted. Among women, HIV prevalence is far higher for those who have ever used condoms (42.7%) than those who have never used them (29.4%). Among men too, prevalence is higher for those who have ever used condoms (30.7%) than those who have never used them (17.6%). Condoms protect against sexually transmitted HIV, not non-sexually transmitted HIV, a subtlety apparently lost on proponents of the sexual paradigm, and mass male circumcision programs.
Despite the best efforts of the HIV industry to find one, there is no unified theory of HIV transmission. It is not all transmitted through heterosexual sex and it is not all transmitted through non-sexual routes. The problem is, we don’t know what proportion is transmitted through sex and what proportion is transmitted through non-sexual routes. Some prevention interventions may work if guided by accurate data about how people are infected with HIV, which people and where. But in the absence of that data the bulk of transmissions will remain unaddressed. Mass male circumcision programs are not even vaguely targeted and only address sexual transmission, so they are irrelevant to the majority of people.